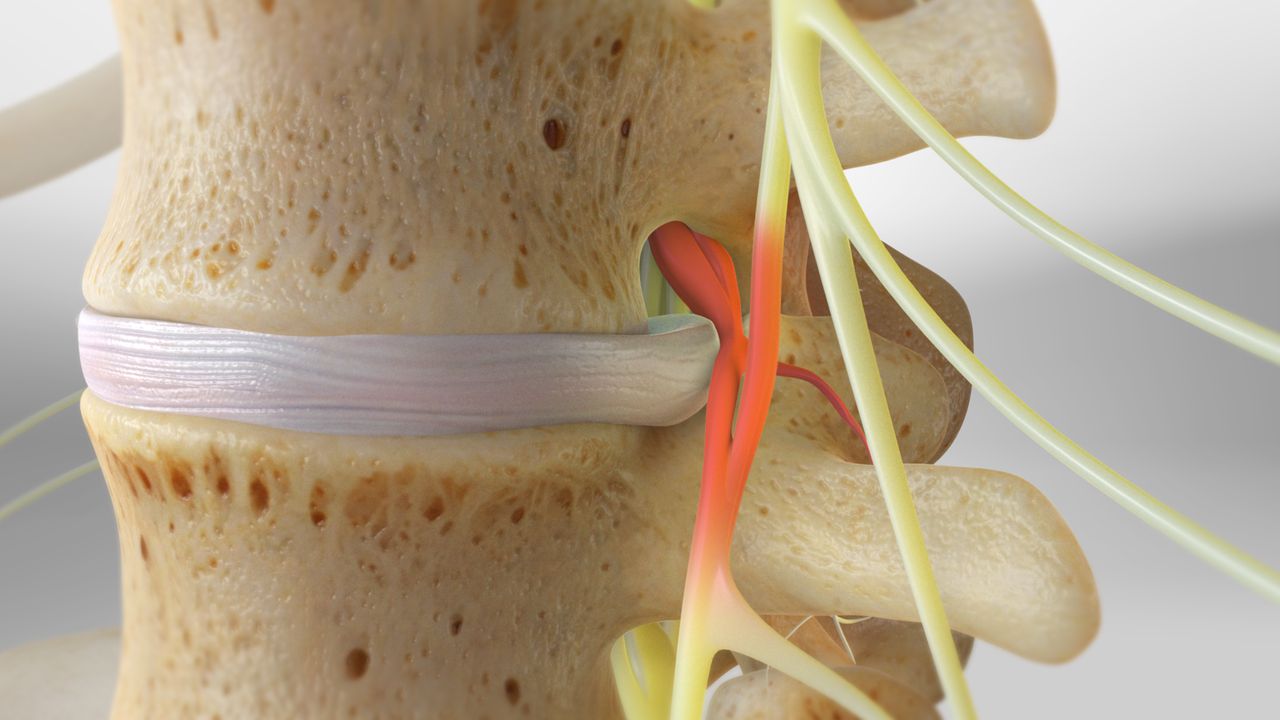
Disc prolapse, also known as a herniated or slipped disc, occurs when the soft, gel-like center of a spinal disc pushes through a tear in the tougher outer layer. This condition can occur in any part of the spine but is most common in the lower back (lumbar spine) or neck (cervical spine). The displaced disc can put pressure on surrounding nerves, leading to pain, numbness, weakness, and other symptoms in the arms or legs. Disc prolapse is often caused by age-related degeneration, but it can also result from sudden injury or repetitive strain. Early diagnosis and treatment are key to managing the condition and preventing long-term damage.
The symptoms of a disc prolapse vary depending on the location of the herniated disc and the extent of nerve compression. Common signs include back pain, radiating pain in the limbs (sciatica), tingling or numbness in the extremities, and muscle weakness. In some cases, a disc prolapse may not cause any noticeable symptoms, especially if the herniation is small and does not press on a nerve. However, when the disc material irritates nearby nerves, it can lead to significant pain and discomfort. A thorough examination and imaging studies, such as MRI or CT scans, are typically required to confirm the diagnosis and assess the severity of the prolapse.
Treatment for a disc prolapse generally starts with conservative methods. Rest, physical therapy, and pain management through medications like NSAIDs (nonsteroidal anti-inflammatory drugs) are common first-line treatments. In some cases, spinal injections of corticosteroids may be recommended to reduce inflammation and relieve pain. Most individuals with a disc prolapse experience significant improvement with non-surgical treatment. However, if conservative methods fail to provide relief, or if the prolapse leads to severe symptoms such as loss of bladder or bowel control, surgery may be required to remove or repair the herniated disc.
Surgical options for disc prolapse include procedures such as microdiscectomy, in which a portion of the herniated disc is removed to relieve pressure on the affected nerve. In more severe cases, a spinal fusion may be necessary to stabilize the spine and prevent further damage. While surgery is typically reserved for cases that do not respond to conservative treatment, it can provide significant relief for patients suffering from debilitating pain and neurological symptoms. Postoperative care involves rehabilitation and physical therapy to strengthen the muscles and improve flexibility, helping the patient recover and prevent future injury.
In conclusion, a disc prolapse is a common spinal condition that can cause significant pain and discomfort due to nerve compression. While many cases improve with non-surgical treatment, more severe cases may require surgical intervention. Early diagnosis and appropriate management are essential to preventing long-term complications, and patients are encouraged to engage in preventive measures such as regular exercise, good posture, and proper lifting techniques to reduce the risk of disc prolapse. With the right care and treatment, most individuals can recover and resume their normal activities without ongoing issues.